Interview with Dr. Rémi Gauthé and Dr. Vianney Gilard, spine surgeons, Centre Normandie Rachis, Clinique Saint-Hilaire, Rouen, France.
Clinique Saint-Hilaire is a medical and surgical institution in which the technical facilities are managed by multidisciplinary teams structured into three key divisions: medical and surgical division, cardiovascular division and cancer division.
In 2021, the medical and surgical division was strengthened by the incorporation of the Centre Normandie Rachis spine surgery practice. This practice comprises five surgeons who provide comprehensive management of spinal disorders affecting adults and children.
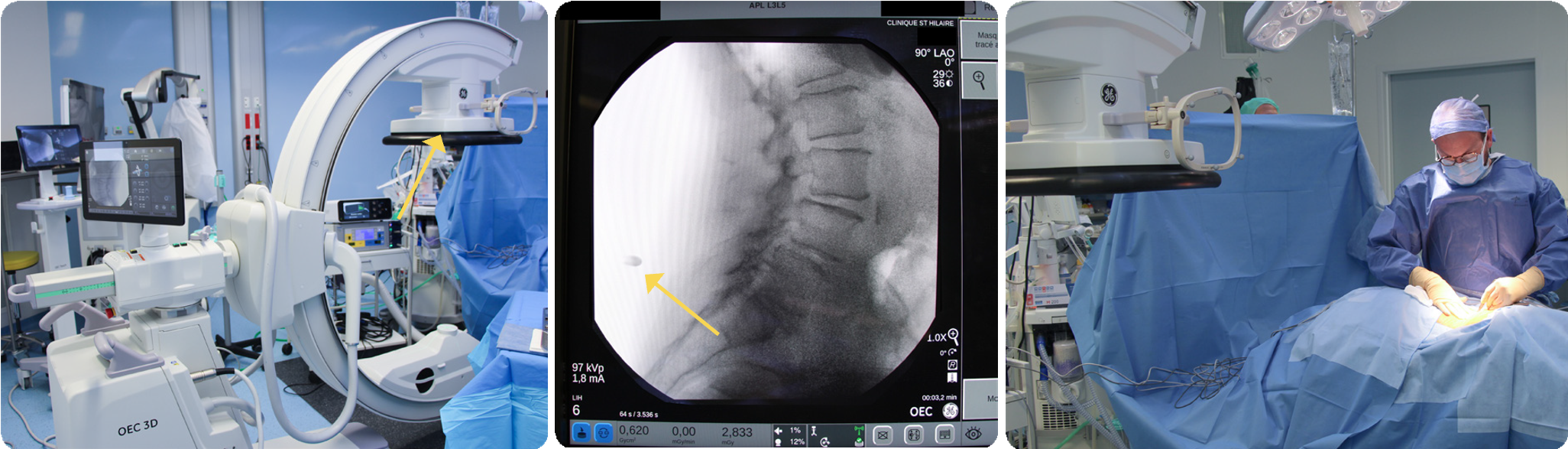
As part of the incorporation of Centre Normandie Rachis, an operating room was created to include a 3D imaging C-arm paired with neuronavigation. After testing different equipment, the center opted for the OEC 3D C-arm with integrated Brainlab Kick® navigation (Brainlab, Munich - Germany). Here, Drs. Gauthé and Gilard share their experience with 3D imaging and integrated neuronavigation after one year of use.
Dr. Rémi Gauthé is an orthopedic and trauma surgeon who specializes in spine surgery. After obtaining his medical degree from Université Paris-Descartes, he completed his clinical training in orthopedic surgery and traumatology at Rouen University Hospital–Charles Nicolle.
After working for four years as a resident, then for a year and a half as a hospitalpractitioner at Rouen University Hospital, he joined Centre Normandie Rachis at Clinique Saint-Hilaire in November 2021. Dr. Gauthé is a member of SOFCOT (Société Française de Chirurgie Orthopédique et de Traumatologie – French Society for Orthopedic Surgery & Traumatology) and SFCR (Société Française de Chirurgie Rachidienne – French Society for Spine Surgery). He is also a member of the French College of Orthopedic Surgeons, which manages the training of interns. Dr. Gauthé belongs to the Spine Research Community (SRC), which brings together 35 private physicians working together on a collaborative medical and clinical research project on the benefits associated with spine surgery.
Could you describe how Centre Normandie Rachis is set up at Clinique Saint-Hilaire?
Dr. Gilard: Clinique Saint-Hilaire is a private family-run clinic owned by the Martin family. It is an independent institution committed to quality of care and quality of work life. This is clearly seen in the clinic’s management, operations and focus on people. The clinic’s moderate size enables it to operate more efficiently. Staff members know each other and work together as a team. The clinic has about 100 practitioners. There are 220 beds, half of which are dedicated to surgery. In addition, there is an oncology department, intensive care unit, post-acute care unit, cardiac rehabilitation unit and an outpatient unit. The clinic therefore provides a large proportion of regional care in medicine and surgery.
Centre Normandie Rachis is a nominal partnership that brings together five spine surgeons from a variety of backgrounds and that delivers comprehensive care for all spinal disorders affecting adults and children. Our group includes one pediatric orthopedic surgeon, two adult orthopedic surgeons who specialize in spine surgery and two neurosurgeons.
I want to stress that we are particularly well equipped and set up at the clinic. Since my arrival, I have been able to use OEC 3D C-arm, an operating microscope, a Cavitron® aspirator, which is used to resect tumors in neurosurgical procedures, and other modern equipment. We are equipped in much the same way as a teaching hospital, which benefits both the staff and patients.
Dr. Gauthé: Since I arrived at the clinic in November 2021, with my colleagues we have been developing the surgical management of spinal disorders in adults and musculoskeletal conditions in children and adolescents. We created a practice that previously did not exist. The clinic’s management made the decision to build a modern operating room dedicated to spine surgery. As a result, the clinic now has equipment specifically intended for use in this facility, such as imaging and navigation systems and the operating table. We submitted a list of the equipment required for our practice, and the clinic then issued a call for tenders, after which we carried out tests and selected our equipment. It is in this context that we chose OEC 3D for the 2D and 3D imaging necessary for our procedures.
We continue to work on building our facility in terms of operating room equipment, as well as the development of our patient consultation, namely communication with referring physicians who send us treatments. I have also started to take on a number of responsibilities regarding radiation safety and the operating room. The practitioners are involved in different areas at the clinic, such as quality, the users’ committee, the infection committee and accreditation.
Within your practice, what are your requirements in terms of 2D and 3D imaging?
Dr. Gauthé: Generally, all our procedures require either 2D or 3D imaging in the operating room. We perform very few surgical procedures without 2D fluoroscopic imaging because we routinely check the spinal level at which we are operating.
Navigation and 3D imaging are not required for all procedures. Our practice is growing and is in its startup phase. We currently treat around four to five patients per day, over four days a week.
Most of the procedures involve lumbar spine fusions and lumbar and cervical disc herniations, which account for about a third of the total volume.
With regard to the use of imaging, 3D guidance is routinely used in procedures involving the insertion of lumbar implants. This means that we do not always use navigation, but we do use volumetric imaging to check the placement of implants.
2D fluroroscopic image of lumbar spine in lateral view to check the spinal level.
We use navigation alongside 3D acquisition for lumbar spine surgery when we anticipate difficulties: for example, when we know that there is extensive scoliosis, short pedicles or anatomy that is significantly altered due to extensive osteoarthritis.
Therefore, when we expect difficulty from the outset in inserting the screws, we use the navigation system. Navigation is not routinely used. In cervical spine surgery, we never use navigation; instead, we use 2D imaging control in antero posterior and lateral views. Exceptionally, we may use 3D imaging. In this case, it is very easy with OEC 3D to switch from 2D imaging to 3D imaging. That is why the C-arm remains permanently available for use in our operating room.
“I think that 2D/3D imaging will become widely used even if only for 3D guidance.” Dr. Vianney Gilard
Dr. Gilard and Dr. Gauthé preparing OEC 3D for the 3D acquisition
Lastly, pedicle screw implantation represents the majority of our activity. This is a procedure in which 3D imaging guidance is the only way of ensuring that the implants are positioned correctly, that the screw is not in contact with a nerve and that it is definitely in the right place. This is what we look at when we perform an intraoperative 3D imaging with
OEC 3D.
In the future, I think that imaging will always be necessary, if only to check the spinal level.
Dr. Gilard: Intraoperative 3D imaging has become our new standard. Today, it is unimaginable to insert an implant without 3D guidance, especially when we are fortunate enough to have the OEC 3D C-arm at our disposal.
Practically speaking, 2D imaging has its limitations, even from a purely medical perspective. This means that if a patient is relatively heavyset, you might not be able to see some implants using 2D imaging. There are also some anatomical areas that cannot be accessed with 2D imaging. However, 3D volumetric imaging provides a comprehensive solution to this problem, making it possible to analyze multiplanar views of large-volume reconstructions and enabling us to view the anatomy behind implants. This is also useful when treating nerve root compression, i.e., removing bone or osteoarthritis that is compressing a nerve root. This is not the most common occurrence, but we can check the quality of our decompression: we view the section of bone we made using forceps, and we can make an estimate to determine whether it is sufficiently clear of the nerves. We learned how to assess nerve compression using a preoperative scan and can now do this using volumetric imaging obtained intraoperatively with OEC 3D.
Another issue to consider is radiation safety. With 2D imaging, lead aprons provide protection, but most of the time, we remain in the room during the imaging process, albeit at a distance. By contrast, 3D imaging with OEC 3D coupled with navigation makes it possible to produce a series of volumetric images with relatively low irradiation, while we remain out of the room. The rest of the procedure then involves little or no radiation, which offers long-term radiation safety to us and other staff members.
In parallel with this, there is a place for navigation, and there will always be a need for direct view imaging, especially endoscopic spine surgery, which is becoming more common. Today endoscopic spine surgery requires 2D imaging to triangulate the position of the endoscope in the treatment of disc herniation. In the future, endoscopy might be navigated with 3D imaging.
Can you explain to us the benefits of OEC 3D integration with Brainlab navigation for your procedures?
Dr. Gauthé: In our surgical technique we use the bare minimum of navigated tools, i.e we work primarily with the navigated locator stylet. We position the screws according to the free-hand technique, then we check their position using OEC 3D intraoperative volumetric imaging.
As with all other screw placement techniques, we work by touch and by controlling the force that we place on the instrument. For me, it is important to control the manual sensation applied to the instruments, to be able to adapt to the feel of the technique instead of relying on automated instruments.
Therefore, we prefer to use the navigation system to identify an entry point and establish the direction of the screws, then to check our technique using OEC 3D imaging.
Navigation is an undeniable aid, especially in the case of complicated screw implantation procedures.
Navigation ensures a more precise and safer technique, making it possible to insert screws on the first attempt when the anatomical points of reference are accurate.
Generally, we use navigation if the preoperative imaging suggests that implantation may be difficult, for example, when there are vertebrae that are slightly twisted, short pedicles or significant alteration of the surface where a lot of bone has formed and the anatomical landmarks are hard to identify.
Dr. Vianney Gilard is a neurosurgeon. Originally from Normandy, he studied medicine and completed his clinical training in neurosurgery at Rouen University Hospital–Charles Nicolle. During his clinical training, he specialized in pediatric neurosurgery and spine surgery and completed two placements: one at Necker– Enfants Malades University Hospital in Paris and the other during his postdoctoral fellowship at Great Ormond Street Hospital for Children NHS Foundation Trust in London. He spent three years working as a resident at Rouen University Hospital in spine surgery and general cranial and pediatric neurosurgery. He then worked as a lecturer and hospital practitioner at Rouen University Hospital for two years. Dr. Gilard joined Clinique Saint-Hilaire in September 2022.
Dr. Gilard is a member of the SFCR, SFNC (Société Française de Neurochirurgie – French Society of Neurosurgery) and the Spine Research Committee (SRC), through which he carries out fundamental and clinical research projects with his associates. Currently, he is focusing on spinal treatments in adult patients and retains an associate position at Rouen University Hospital in pediatric neurosurgery.
Dr. Rémi Gauthé reviewing the final control images of the procedure on the OEC 3D workstation using the 3D volume viewer.
“A decisive factor in the selection of OEC 3D was the volumetric image reconstruction method. I like having the ability to easily take oblique slice images in the screw axis, the vertebral axis, exactly as I used to do with a CT scanner in multiplanar reconstruction (MPR) mode.” Dr. Vianney Gilard
Dr. Gilard: Navigation should be viewed as an aid to identify anatomical landmarks and to facilitate our practices, rather than as a replacement for them. By inserting the screw in a single step, without damaging any anatomical structures, we maintain the stability of the implant. This ensures efficiency and patient safety.
Furthermore, we considered radiation safety thoroughly since our specialty involves a high level of exposure. Our patients undergo surgery once, perhaps twice, in their lifetimes and are exposed to some X-rays. For us, we see as many as ten patients per week over a 35-year career. There is a real need to reduce our exposure to X-rays. When we use a navigation system, the staff and surgeons leave the room during the 3D acquisition, thereby significantly reducing their exposure.
For some procedures lasting up to three hours, this prevents us having to wear lead aprons, which has significant practical benefit. When we use navigation in the procedure, we take front and lateral views, we leave the room during 3D acquisition and we do not have to wear a lead apron during the procedure.
Dr. Gauthé: The integration of the Brainlab navigation system with the OEC 3D C-arm is an additional benefit. The communication between the camera and the C-arm makes it possible to signal and suspend the trackers if the navigation trackers are not correctly located by the camera. If the navigation system were not integrated with the C-arm, we might proceed to the acquisition, realizing once the acquisition was complete that the navigation trackers were not in view of the camera, meaning that we would have to perform the 3D acquisition again. The communication between the navigation system and the imaging system is a kind of safety measure ensuring that we don’t perform a 3D acquisition that cannot be navigated. The integration allows the automatic transfer of the 3D images to the navigation computer.
The calibration between the C-arm and the navigation system enables to avoid using an additional tracker on the patient in the 3D volume image. This simplifies the centering of the anatomy of interest in the 3D volume image and enables surgery to be performed with a clearer surgical field.
After using OEC 3D for about one year, which features do you like and use the most?
Dr. Gilard: I find OEC 3D quite user- friendly and intuitive. The OEC Touch control panel menus are simple, and it is easy to select/unselect the various fluoroscopy modes in 2D imaging.
If the patient is thinner, I activate the low dose mode; otherwise, I usually work in standard mode. I only use pulsed mode, which is slightly more irradiating than low dose mode, with larger patients who are more radiopaque. I regularly use the collimation feature, which enables to reduce the radiation field to the anatomy of interest and improves image quality.
The 3D acquisition menu can be accessed at the same menu level as that of 2D imaging. It is easy to switch between 2D acquisition and 3D acquisition. This is simple to do because you can follow the different steps guided by the OEC 3D Setup Assistant.
In addition, the Volume Viewer on the Workstation is easy to use; it is intuitive and touch operated.
Dr. Gauthé: In my practice, for 2D imaging, I usually set the C-arm to low dose mode and pulsed mode at 8 pulses per second. I deactivate low dose mode to see better if the patient is larger. But that is quite rare. I use the preset imaging profiles ‘Spine’ or ‘C-Spine’ depending on the procedure. For a cervical spine procedure, I configure the C-arm using the ‘C-Spine’ imaging profile and I am satisfied with that. For a thoracolumbar spine procedure, I configure the C-arm using the ‘Spine’ imaging profile. I find the image quality perfectly appropriate for carrying out my procedures.
I like the anticollision system located on the detector. It is extremely effective. When performing a simple procedure with 2D imaging, the C-arm is placed under sterile drapes. If the C-arm touches the patient during its rotation, we are not aware of it. The C-arm signals this, and then it stops. We could describe this as a soft stop.
Even if it touches the patient’s arm, it will not roll over it. It stops before that point. It does take up space, but that proves useful, too.
For 3D imaging, there are three acquisition modes: Standard (SD) mode, High Definition (HD) mode and HD+ mode. I usually configure the
C-arm using the HD mode. When the system was installed, we activated the metal artifact reduction (MAR) feature, as well as the noise filter. Recently we have activated the eNR. We do not change these settings because we routinely work with metal implants and these filters enable us to obtain our desired level of image quality.
With the other 3D C-arms that we tested, reading the images was much too complicated.
Dr. Gilard: In the past, I often used a different 3D C-arm, which was very bulky and lacked versatility.
In our practice, we need a versatile 2D and 3D imaging tool. We also wanted the freedom to choose the navigation tool that we coupled it with.
As part of our selection process, we also considered the human support aspect. We did not choose a tool and an imaging system, we chose a team with whom we felt supported and assisted. We could have the best tool on earth, but if there were no customer service, engineers or a good working relationship, it would fail. We think that it works well and that’s why we’re happy to be here with you.
Dr. Vianney Gilard is a paid consultant for GE HealthCare and was compensated for his participation in this testimonial.
The statements by GE HealthCare customers described here are based on their own opinions and on results that were achieved in the customer’s unique setting. Since there is no “typical” hospital and many variables exist, i.e. hospital size, case mix, etc., there can be no guarantee that other customers will achieve the same results. JB25770XX
Case report
OEC 3D workflow if using navigation
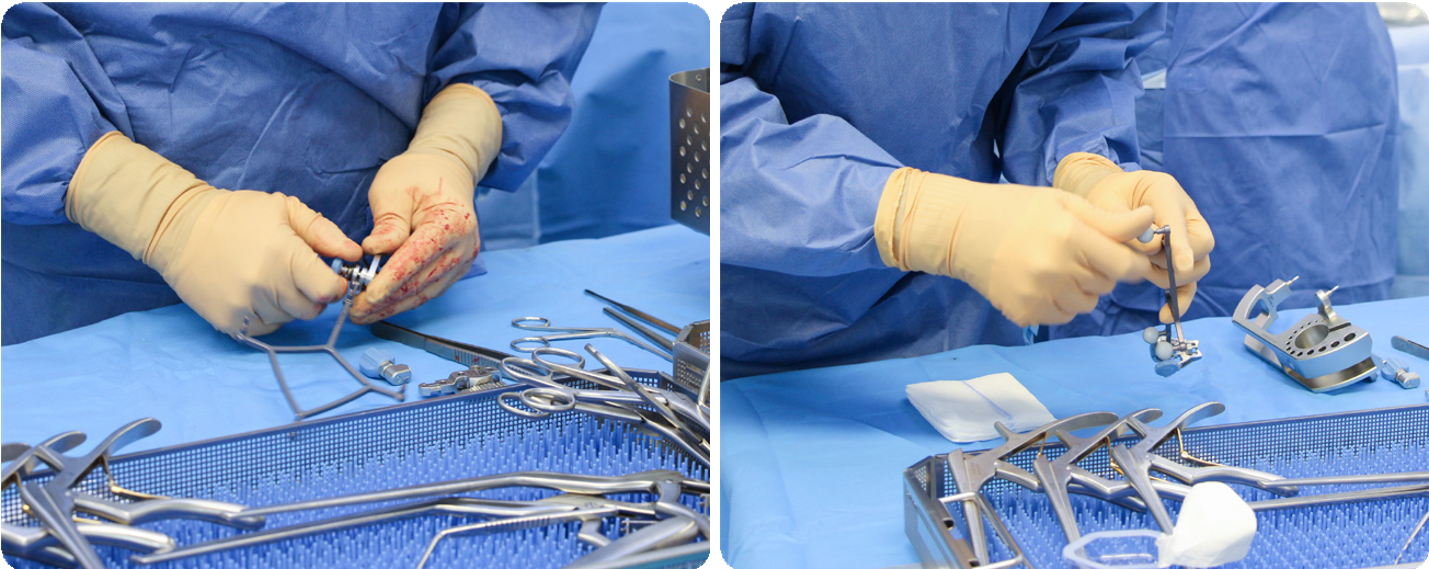
Brainlab Drape link navigation tracker for OEC 3D is fixed on the detector, and Brainlab system is connected to OEC 3D via the integrated navigation port of OEC 3D workstation. A single 2D image is acquired in lateral view over the patient lower back anatomy to identify the incision level necessary to fix the patient pin tracker on the ilium bone. This image is done with the spine imaging profile and standard continuous fluoroscopy. Once the incision is performed, surgeon prepares the navigation patient’s tracker. After draping the equipment, surgeon proceeds to 3D imaging data acquisition.
Brainlab navigation preparation: Patient Tracker
Left image: Drape link for OEC 3D fixed on detector handle.
Center image: Incision level on 2D spine profile.
Right image: Patient incision for patient tracker placement.
Incision level on 2D spine profile
Preparation of patient tracker with its reflective marker spheres.
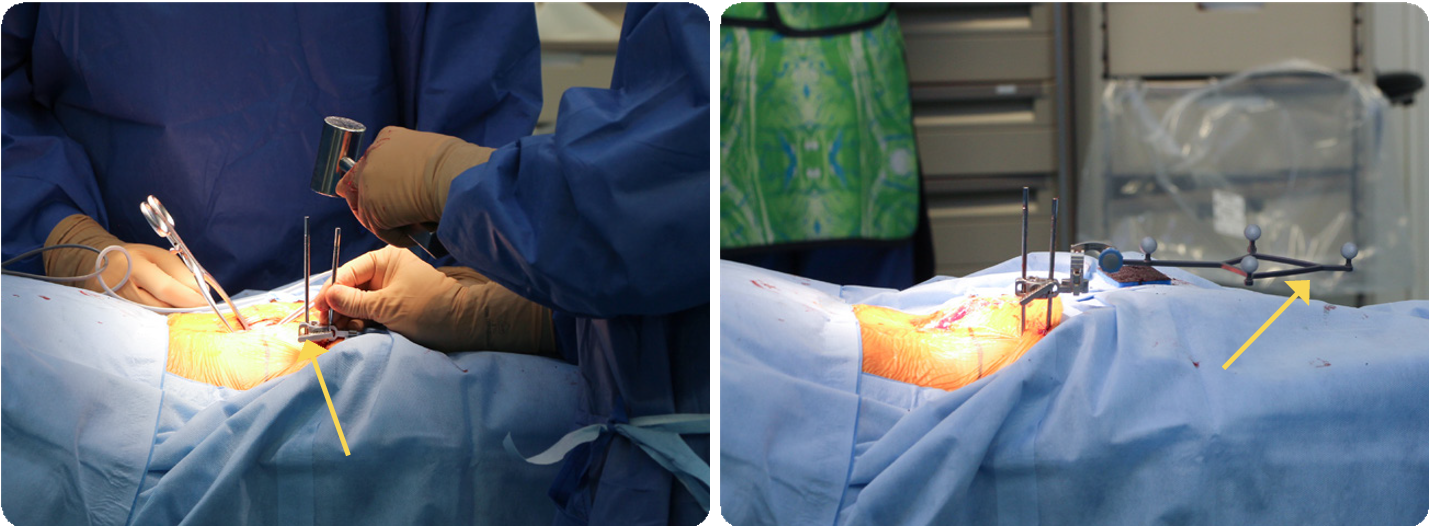
Left image: Fixation of patient tracker pin on the iliac crest. Right image: Attachment of the reference array on patient pin tracker.
OEC 3D preparation: draping
OEC 3D - 3D Setup Assistant
STEP 1: 3D set up
Set up of patient orientation, imaging acquisition mode, dose level and 3D volumetric images reconstruction option. Activation of the connectivity with the integrated Brainlab navigation system.
STEP 2: centering
Anatomy centering in the 3D volume – AP and Lateral view.
STEP 3: collision check
Collision check over 200° rotation starting point at + 130°. All over the 200° rotation, OEC 3D and Brainlab navigation system communicate checking the trackers are visible. During the 3D collision check doctor verifies that the Brainlab navigation systems sees the navigation trackers.
Collision check complete.
STEP 4: imaging
Brainlab camera tracks the C-arm position and the patient position for each image of projection acquired. OEC 3D displays projection images acquired at each degree. OEC 3D completes acquisition of projection images for volumetric image reconstruction up to 200° rotation.
Left image: OEC 3D rotation and exposure stops automatically when the percentage of completion shows 100%. Right image: 3D volumetric images are automatically reconstructed, displayed on OEC 3D workstation, and sent to Brainlab navigation system. Doctor is ready to start navigated surgery.
completion shows 100%.
Lumbar spine fusion
Surgeon working with pointer to identify entry point and direction of the screws to be placed in pedicle.
Pedicle screws are placed with free-hand technique.