Intra-operative imaging for complex endovascular procedure: management of post-stenting complications with OEC 3D
Interview with Dr. Nasser Alwehaibi, head of Vascular Surgery and Chief of the Operating Room at King Fahad Specialist Hospital, Buraydah, Kingdom of Saudi Arabia.
In the north-central part of Saudi Arabia, in the heart of the beautiful province of Al Qassim, the capital Buraydah, historical city renowned for its multicultural festivals, is fully committed to its public hospital King Fahad Specialist Hospital (KFSH).
This 500 bed hospital serves a population of approximately two million people. It covers all medical specialties including surgery, medicine, oncology, obstetrics, and gynecology.
In a spirit of continuous improvement of patient care quality, the surgery department acquired the OEC 3D C-arm as a mobile Hybrid OR (HOR) solution for the vascular surgery team.
Dr. Alwehaibi, head of department of vascular surgery and chief of the operating room shares with us what considerations went into selecting OEC 3D for his routine work and complex vascular procedures.

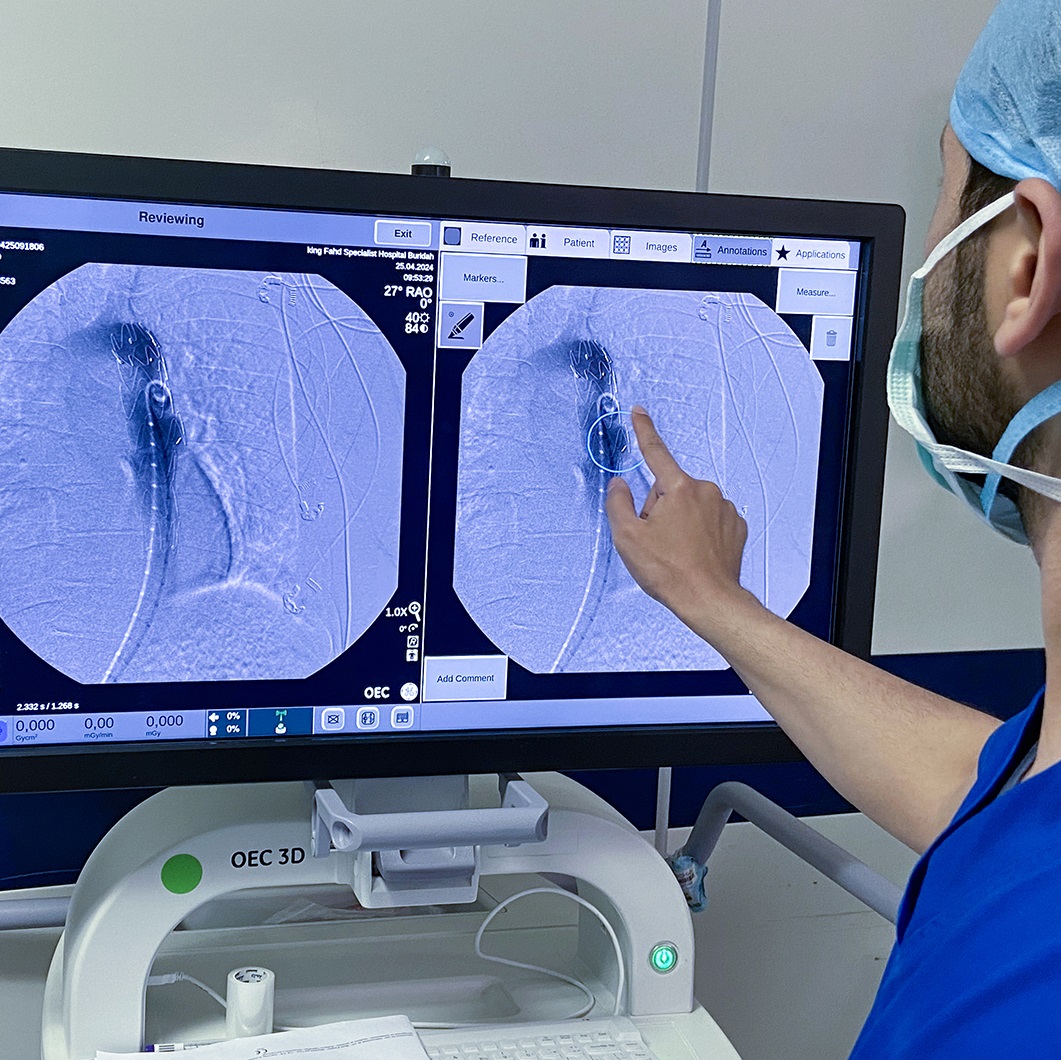
On the left Figure: In the mobile HOR, OEC 3D is positioned next to the patient and the anesthesia workstation is placed next to the patient’s head. The main operator stands to the right of the patient. On the right Figure: Dr. Nasser Alwehaibi highlighting with Digital pen the endoleak in the aneurismal sac of the aorta.
Dr. Alwehaibi’s main incentives to acquire OEC 3D are the advanced techniques and technology in the vascular surgery field. “I felt that with OEC 3D, we could keep up with these evolving endovascular techniques, which make it an exciting and dynamic specialty to pursue.”
Dr. Alwehaibi, can you tell us more about your experience and imaging needs in your work?
“I am Dr. Nasser Alwehaibi, a vascular surgeon with around seven years of experience. I graduated from King Saud University, completed my Saudi Board of Vascular Surgery, and then did a three-year fellowship at King Saud University Hospital.
My professor at King Saud University Hospital, who specializes in arterial vascular procedures, was a significant mentor. His best advice was to always plan ahead of the procedure, or as I say now, ”failure to plan is planning for failure”. ”
“I felt that with OEC 3D, we could keep up with these evolving
endovascular techniques, which
make it an exciting and dynamic specialty to pursue.”Dr. Nasser Alwehaibi
I now work at KFSH as the head of the vascular department with a team of three vascular surgeons, five assistants, and around three residents each year. In the operating room, aside from the anesthesia team, we usually have the operator, an assistant, a scrub nurse, another OR nurse, and a radiology technician.
As we are a tertiary hospital, we use the OEC 3D C-arm for advanced endovascular arterial procedures. These include aorto-iliac, iliac, and lower limb procedures, for which 2D fluoroscopic imaging guidance and control, as well as 3D imaging, are necessary. For our aortic work with TEVAR (Thoracic Endovascular Aortic Repair) and EVAR (Endovascular Aneurysm Repair), in addition to advanced 2D fluoroscopic imaging, we consider that Cone Beam CT (CBCT) imaging mode is mandatory to evaluate post operative complications.”
Dr. Alwehaibi, can you share an example of your work and how you overcome your challenges?
“First, I was looking for a Hybrid OR solution for both endovascular treatment and open surgeries. The most challenging aspect was the limited space I had to work in, so we decided to opt for a mobile 3D C-arm. After evaluation, we were convinced that OEC 3D was the best and only solution that suited me and covered all my needs.
“When I perform preoperative planning, I define all the working projection positions I need for peripheral arteries cannulating, and I save the corresponding C-arm positions to recall them as needed during the operation. Moreover, I am impressed by OEC 3D roadmap capabilities; the images are very precise, and the quality is excellent. This kind of roadmap increases the possibility of successfully crossing and cannulating the anatomy.”
Dr. Nasser Alwehaibi
One of the most difficult situations is arterial cannulation in EVAR (Endovascular Aneurysm Repair) cases, or when trying to cross a stenosis. This is why the image quality (IQ) needs to be precise so that small, short segment stenoses can be seen clearly, ensuring safe practice during endovascular treatment. I can achieve that thanks to the high IQ of the Roadmap mode, using the Digital Pen tool, and the preset positions functions."
What are the fluoroscopy modes and functions that affect image quality?
“Usually, I use the ‘Vascular’ or ‘General HD’ imaging profiles in standard fluoroscopy, subtraction, and roadmap. In some cases, I mix the Live Zoom and magnification modes to obtain the best outcome from both functions.”
“I foresee significant improvements in patient care due to increased financial and manpower support from the government. The trend in medicine is shifting towards subspecialties, minimally invasive procedures, and new technologies in imaging modalities such as OEC 3D, which will likely enhance our activities.”
Dr. Nasser Alwehaibi
 |
Dr. Nasser Alwehaibi is a Vascular and Endovascular Surgeon and the Head of the OR and Anesthesia Department at King Fahd Specialist Hospital in Buraydah, Saudi Arabia. He completed his MBBS at Qassim University in 2012 and earned the Saudi Board in General Surgery in 2018. Dr. Alwehaibi further specialized by completing a Fellowship in Vascular Surgery at King Saud University in 2022. He is passionate about advancing minimally invasive procedures in vascular surgery and is dedicated to adopting and developing new techniques that enhance patient outcomes and recovery. |
Clinical case
73-year-old man with a history of diabetes, hypertension, and ischemic heart disease, presented with severe back pain. Examination and imaging revealed a large, partially thrombosed descending aortic aneurysm. The patient underwent TEVAR, where a stent graft was deployed in the descending thoracic aorta, and the diagnostic angiogram showed a type III endoleak. An emergency reoperation was performed using another stent graft, successfully sealing the endoleak. The patient recovered well post-operation and was discharged with stable vitals.
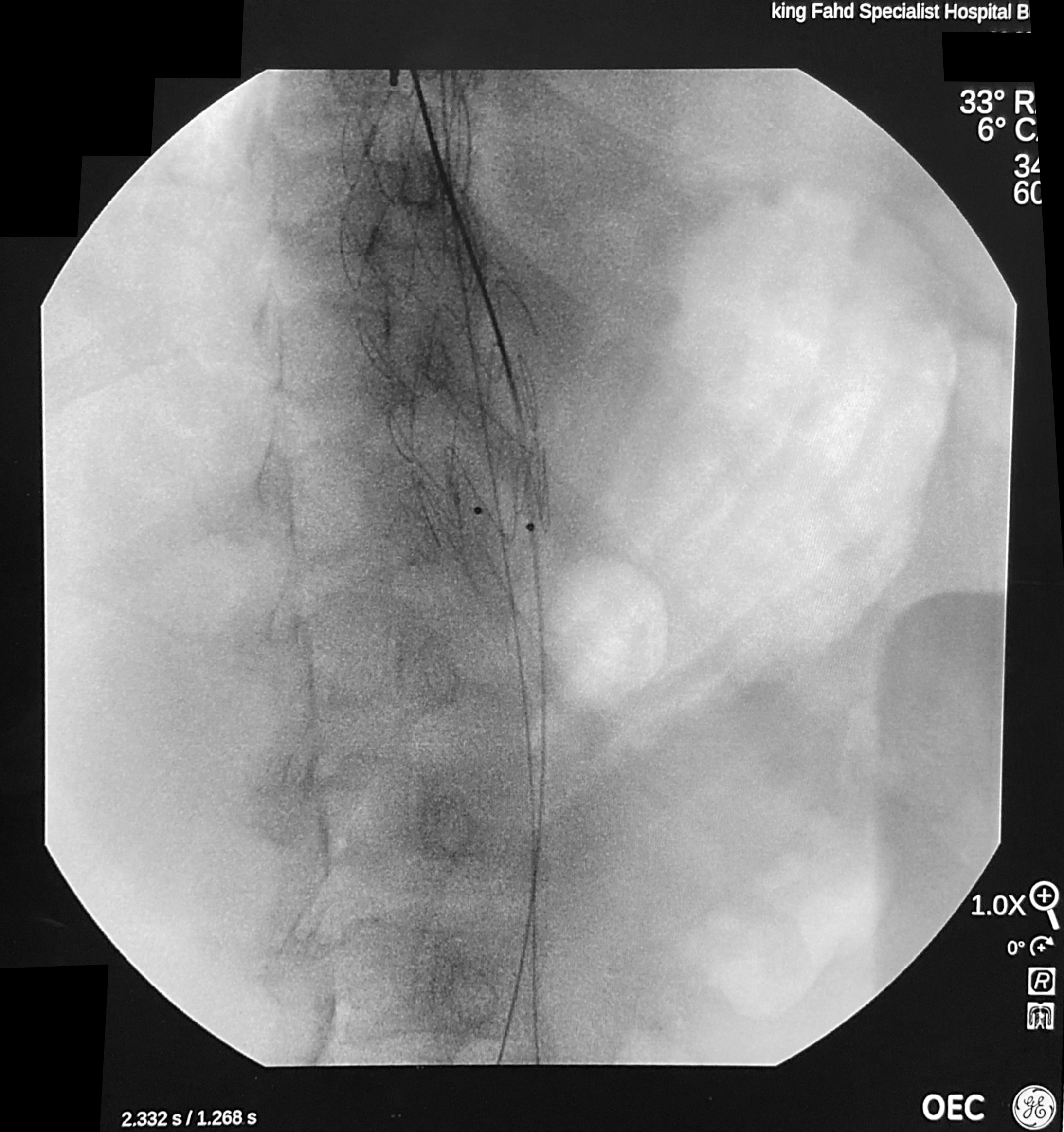
The main challenge was detecting and managing complications. The OEC 3D C-arm was positioned on the patient’s right side with the anesthesia workstation placed at the patient’s head. Vascular access has been performed via the left common femoral artery and a pigtail catheter has been used for endovascular navigation to reach the aortic arch. The device was deployed under fluoroscopic imaging guidance, using the Vascular imaging profile, roadmap, and subtraction imaging modes, with no magnification and no collimation.
1. Digital Subtracted Angiography (left image), non-subtracted fluoroscopic image (right image): visualization of unruptured thoracic aortic aneurysm sac confirming pre-operative diagnostic.
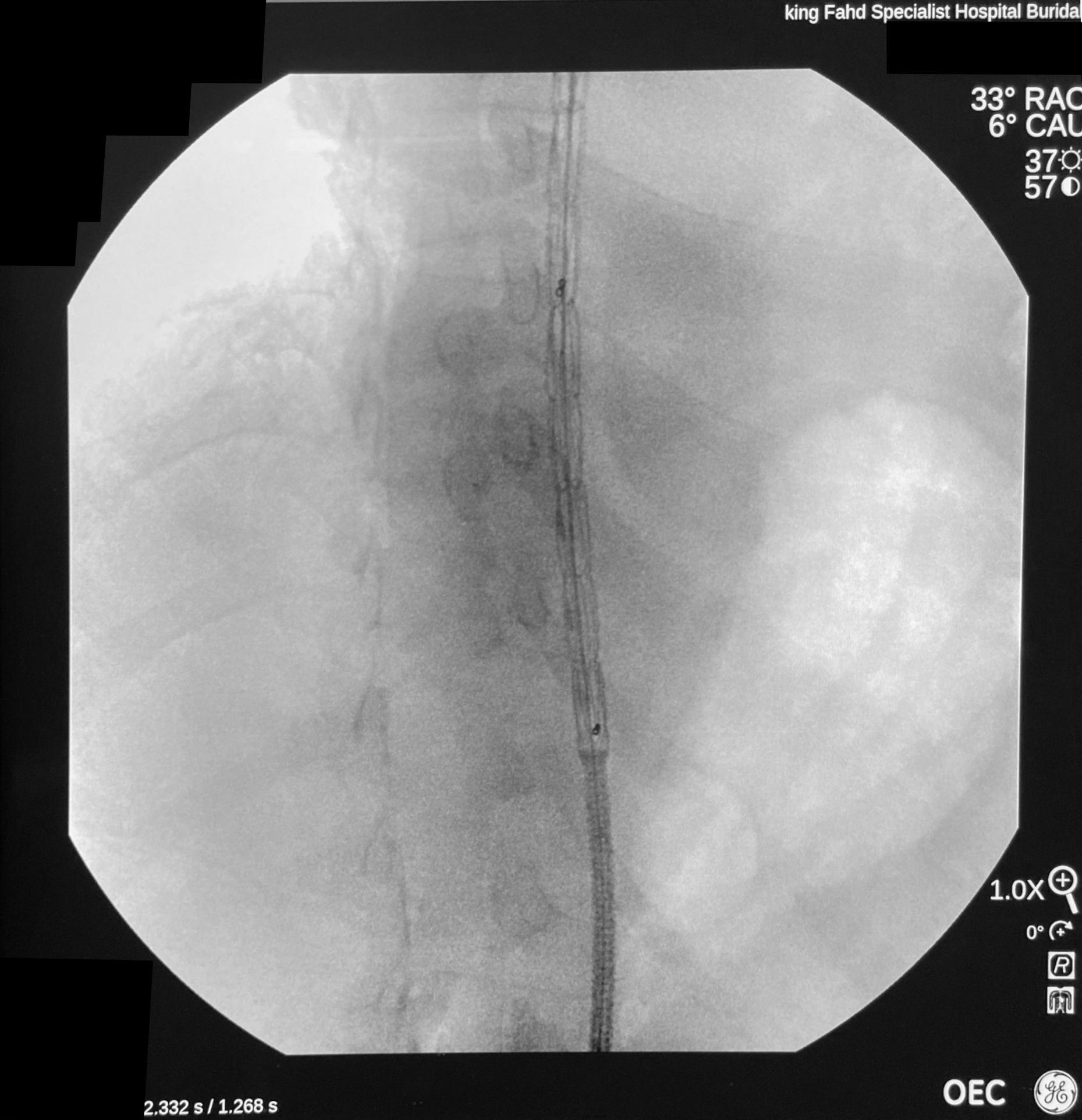
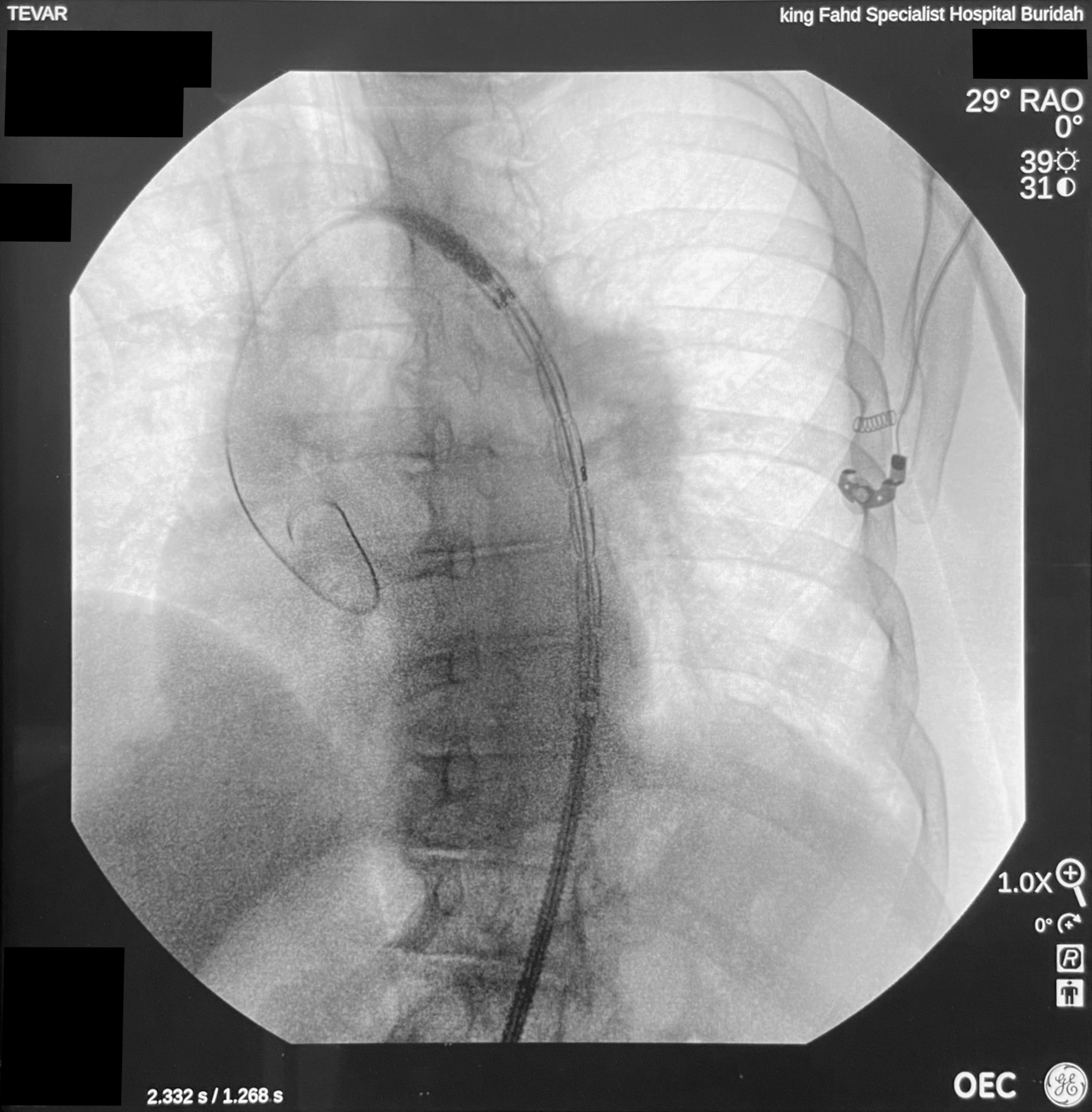
2. Dynamic fluoroscopic images, in Vascular imaging profile, during the placement in the aorta of the delivery sheath containing the thoracic stent graft. Identification of optimal placement of the stent graft vs. aneurismal sac.
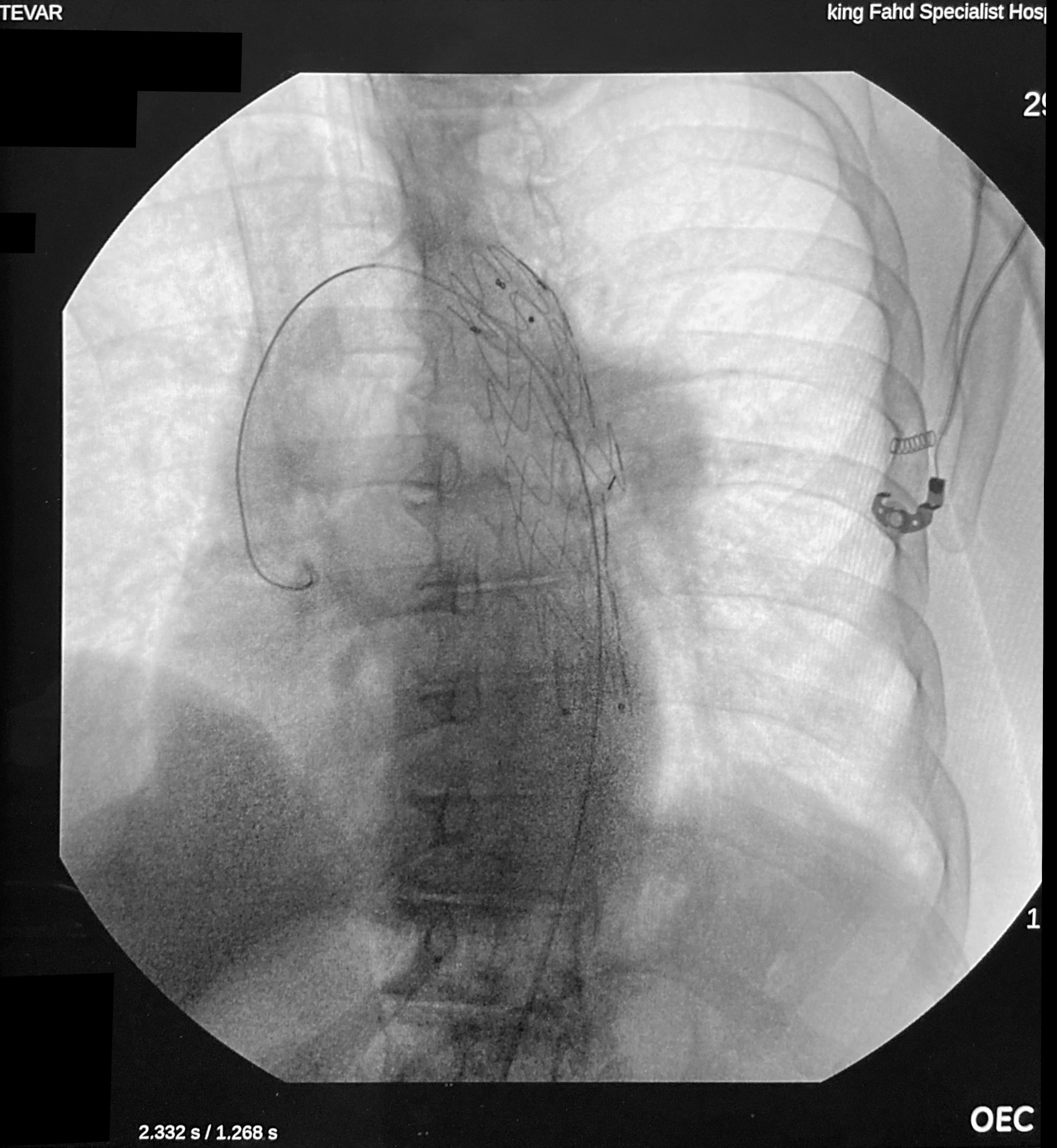
3. Dynamic fluoroscopic image showing the dilatation of the stent graft over the aorta lumen with an endoluminal balloon.
4. Dynamic fluoroscopic images, in Vascular imaging profile, during the control of the placement of the thoracic stent graft. Identification of a leakage defect of the stent towards aneurismal sac.
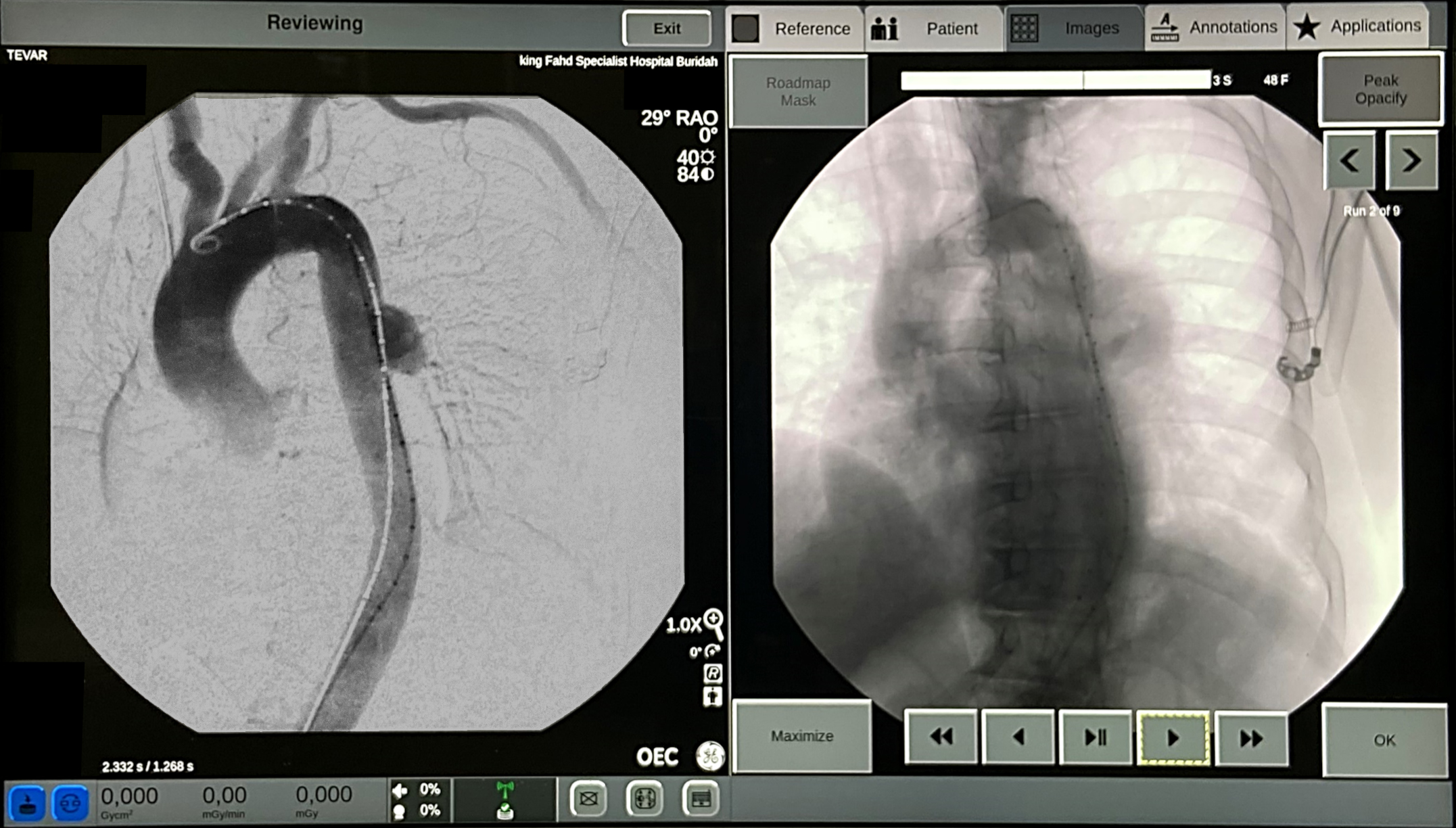
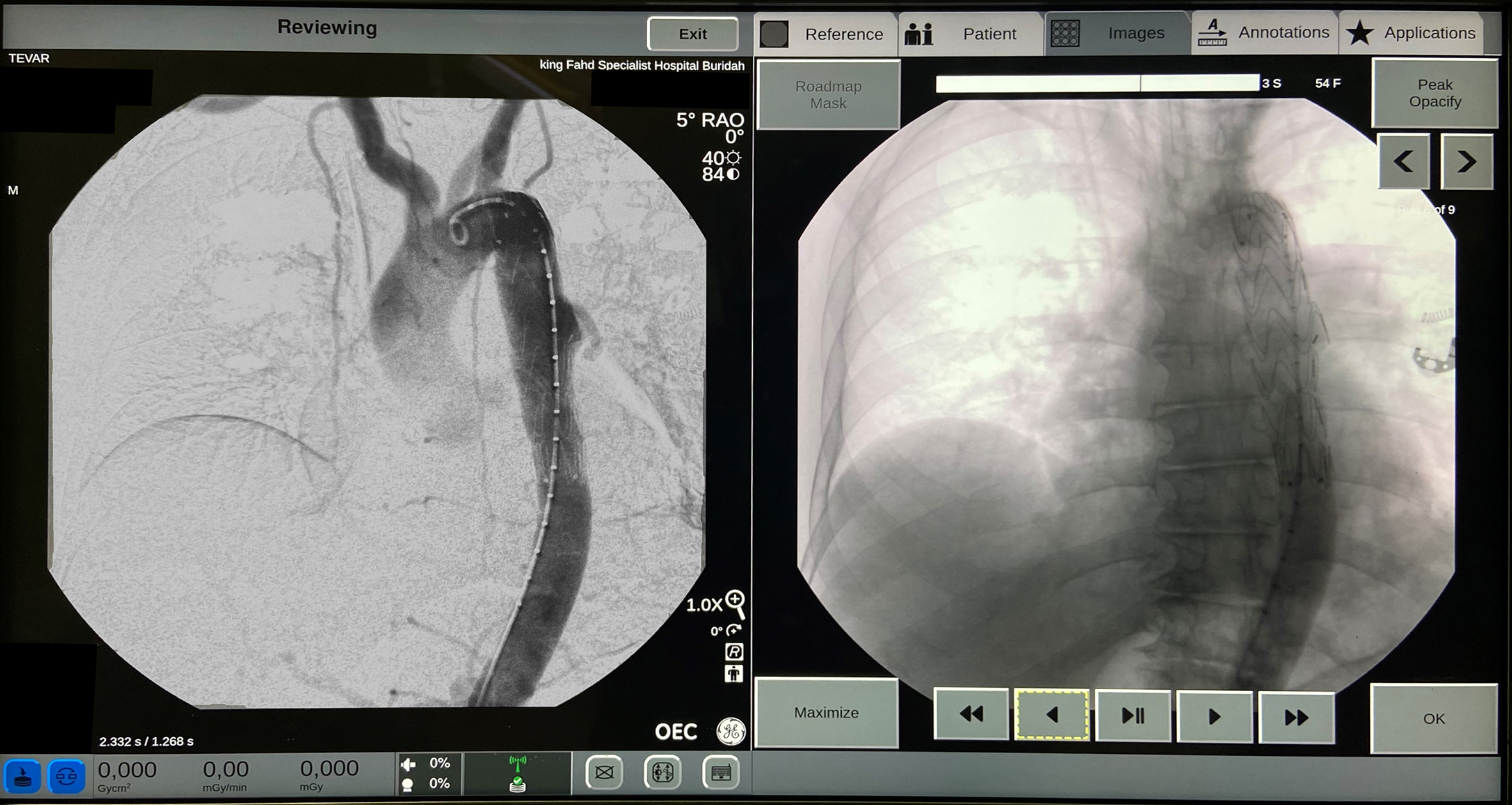
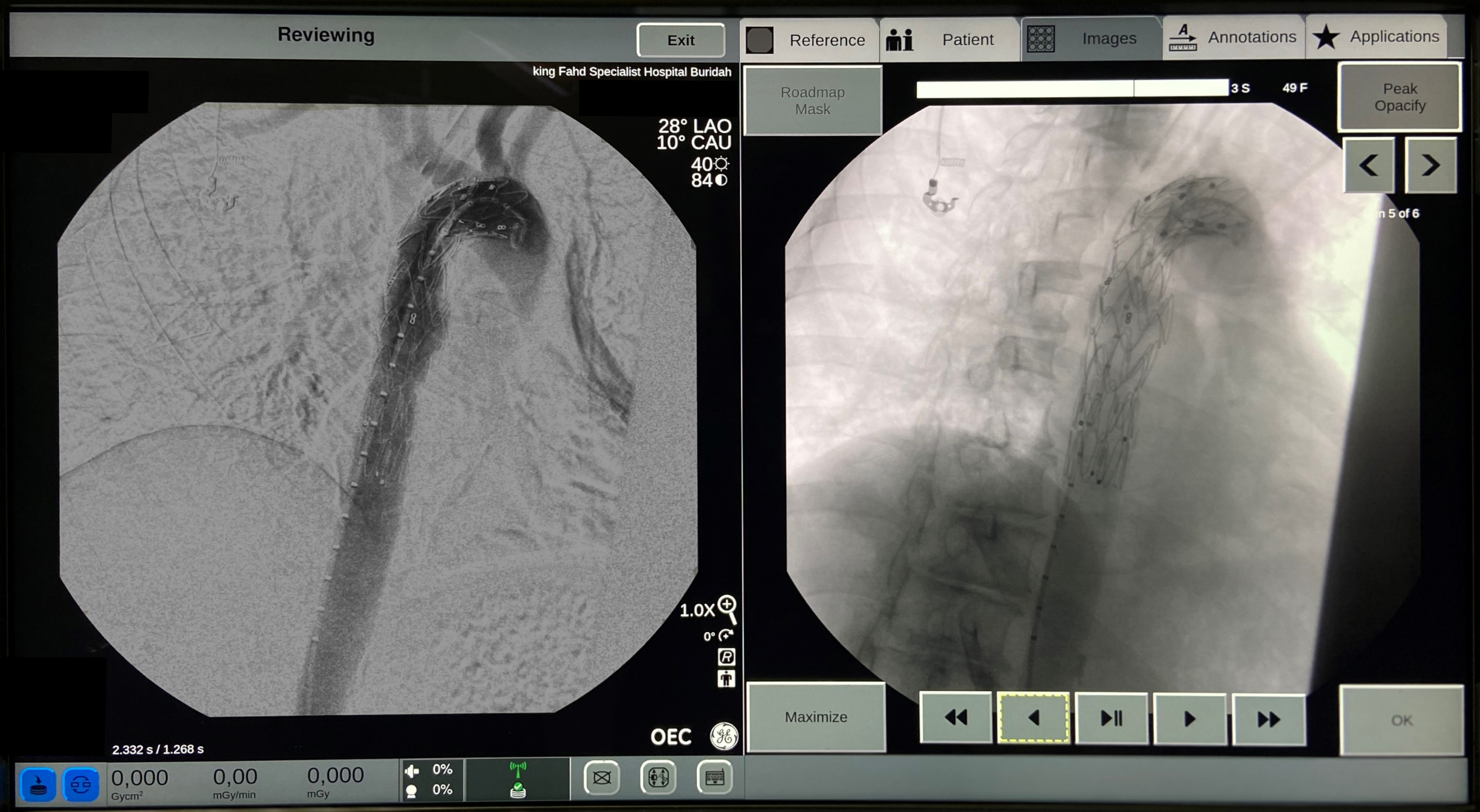
5. Digital Subtracted Angiography (left image), non-subtracted fluoroscopic image (right image): visualization of the endoleak into the aneurysmal – acquisition performed in antero posterior view.
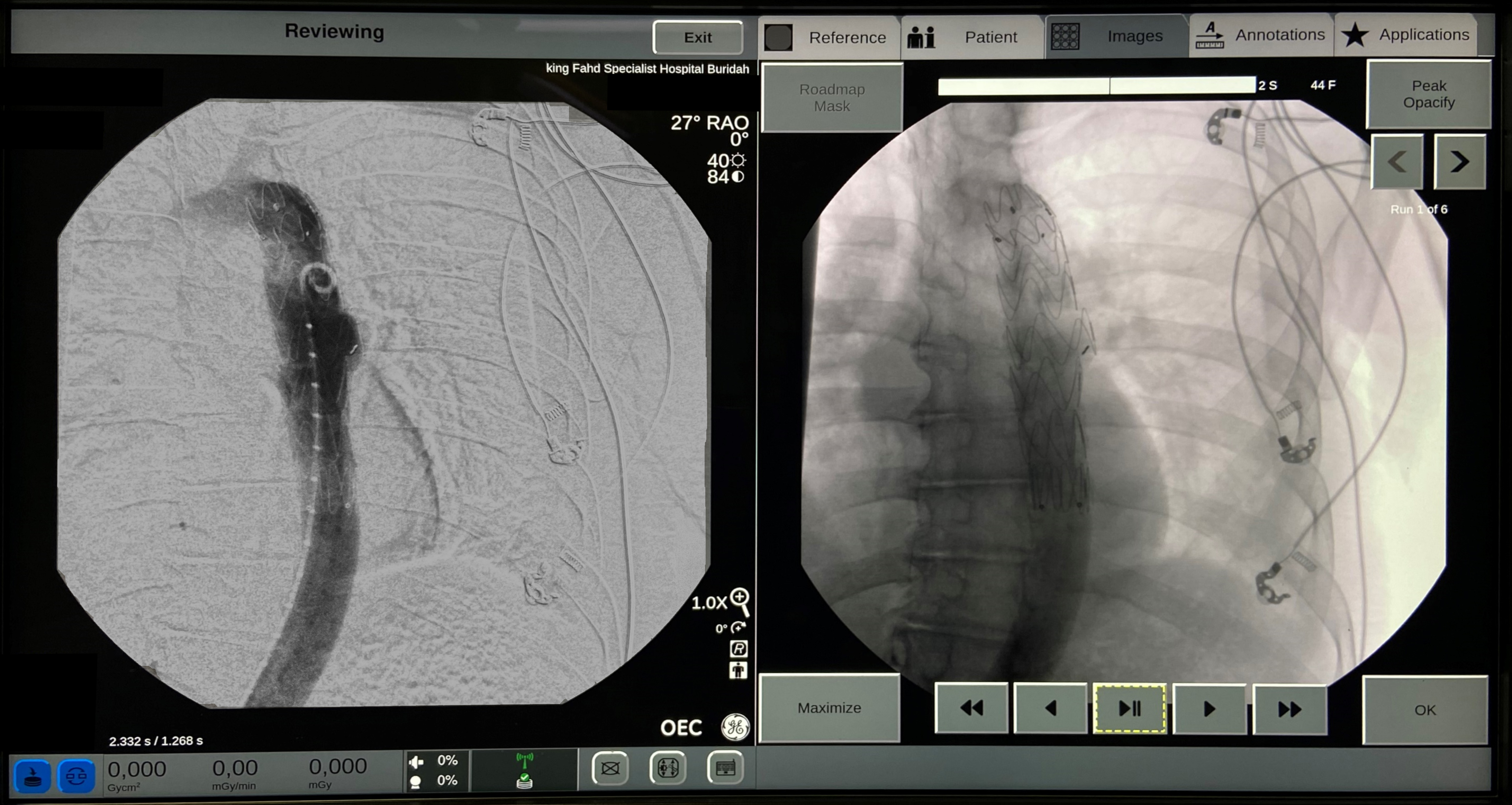
6. Digital Subtracted Angiography (left image), non-subtracted fluoroscopic image (right image): confirmation of the post stenting endoleak into the aneurysmal lumen – acquisition performed in right oblique view of about 30 degrees.
7. Digital Subtracted Angiography (left image), non-subtracted fluoroscopic image (right image): confirmation of the post stenting endoleak into the aneurysmal lumen – acquisition performed in antero posterior view.
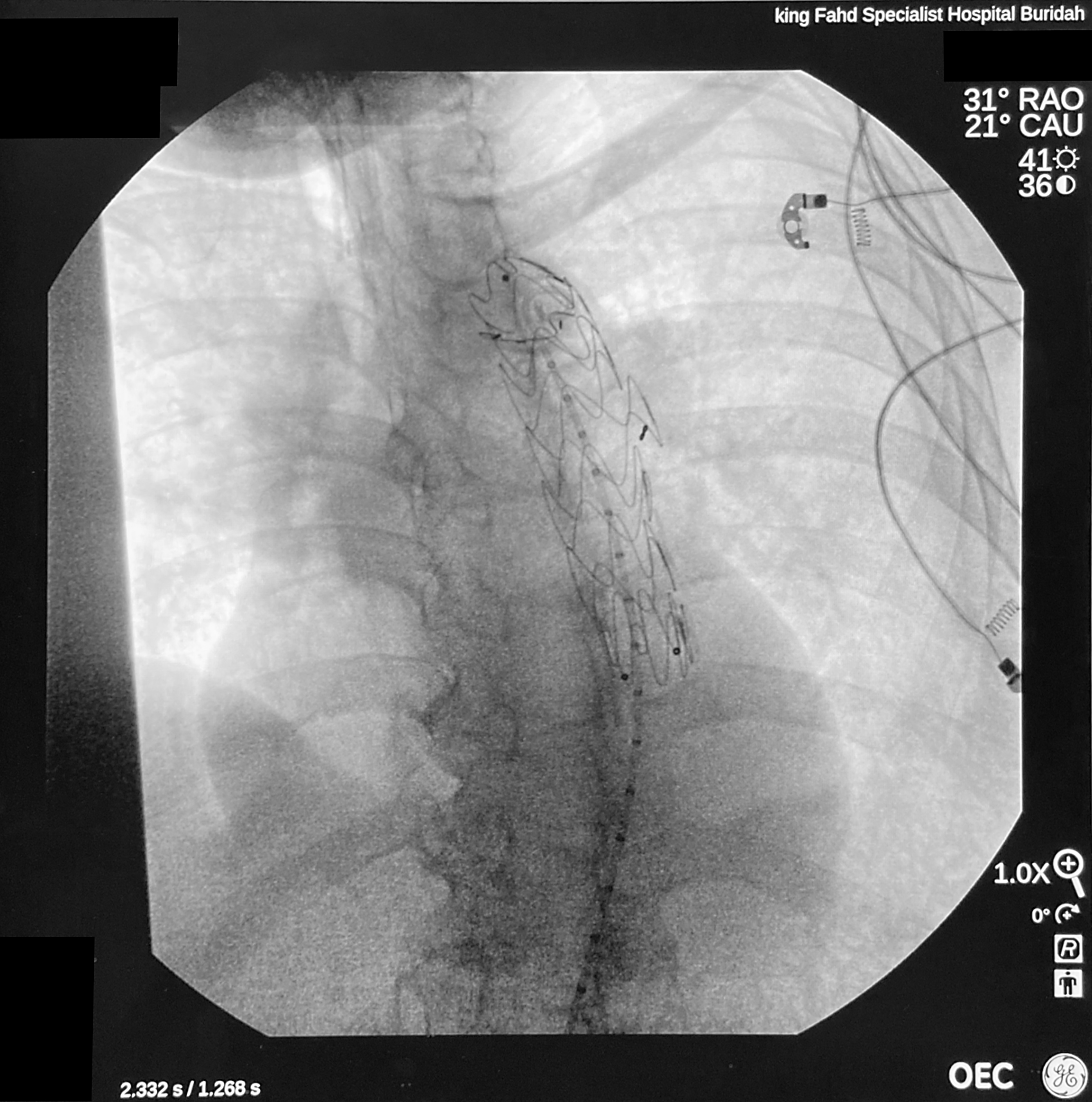
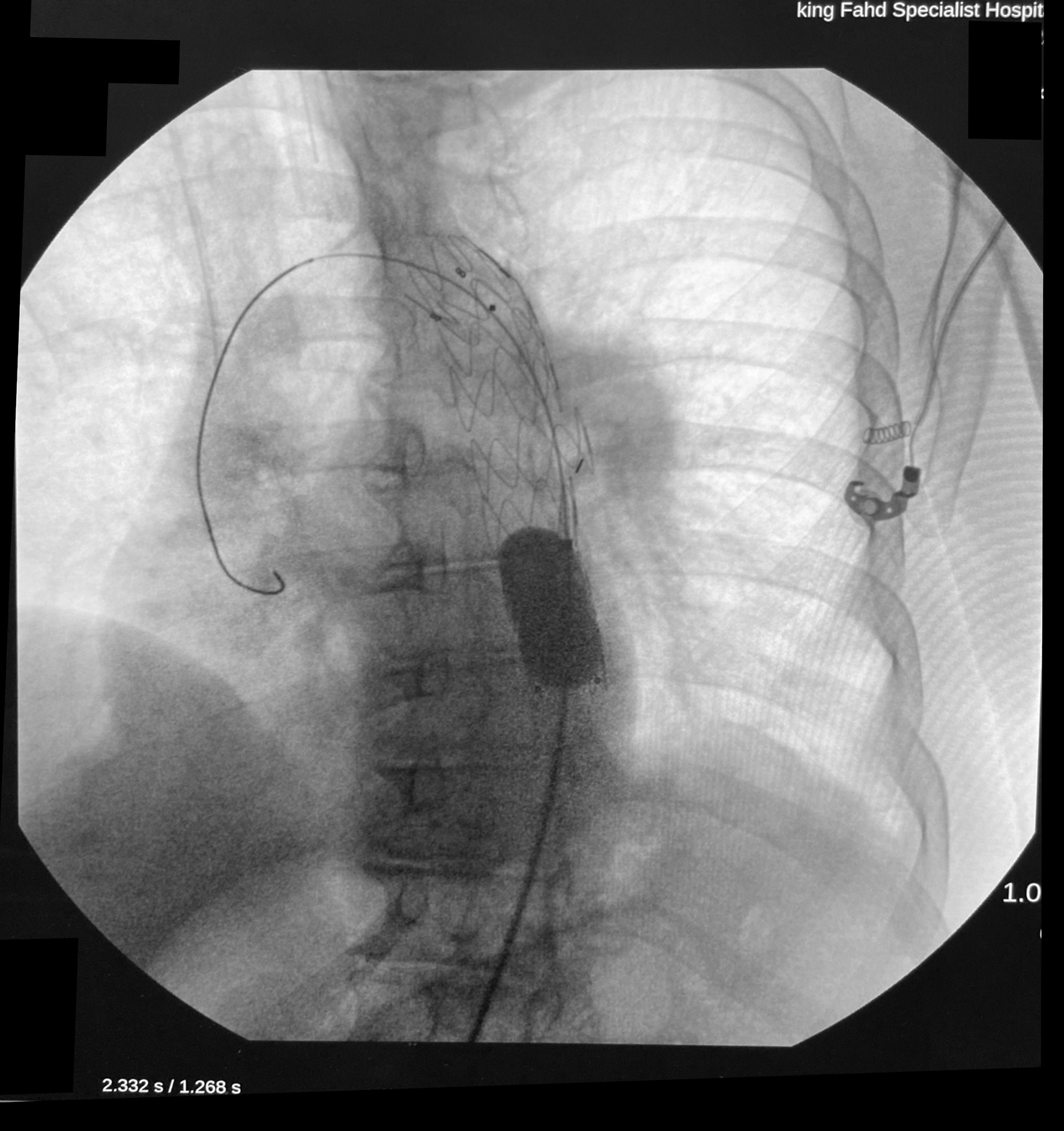
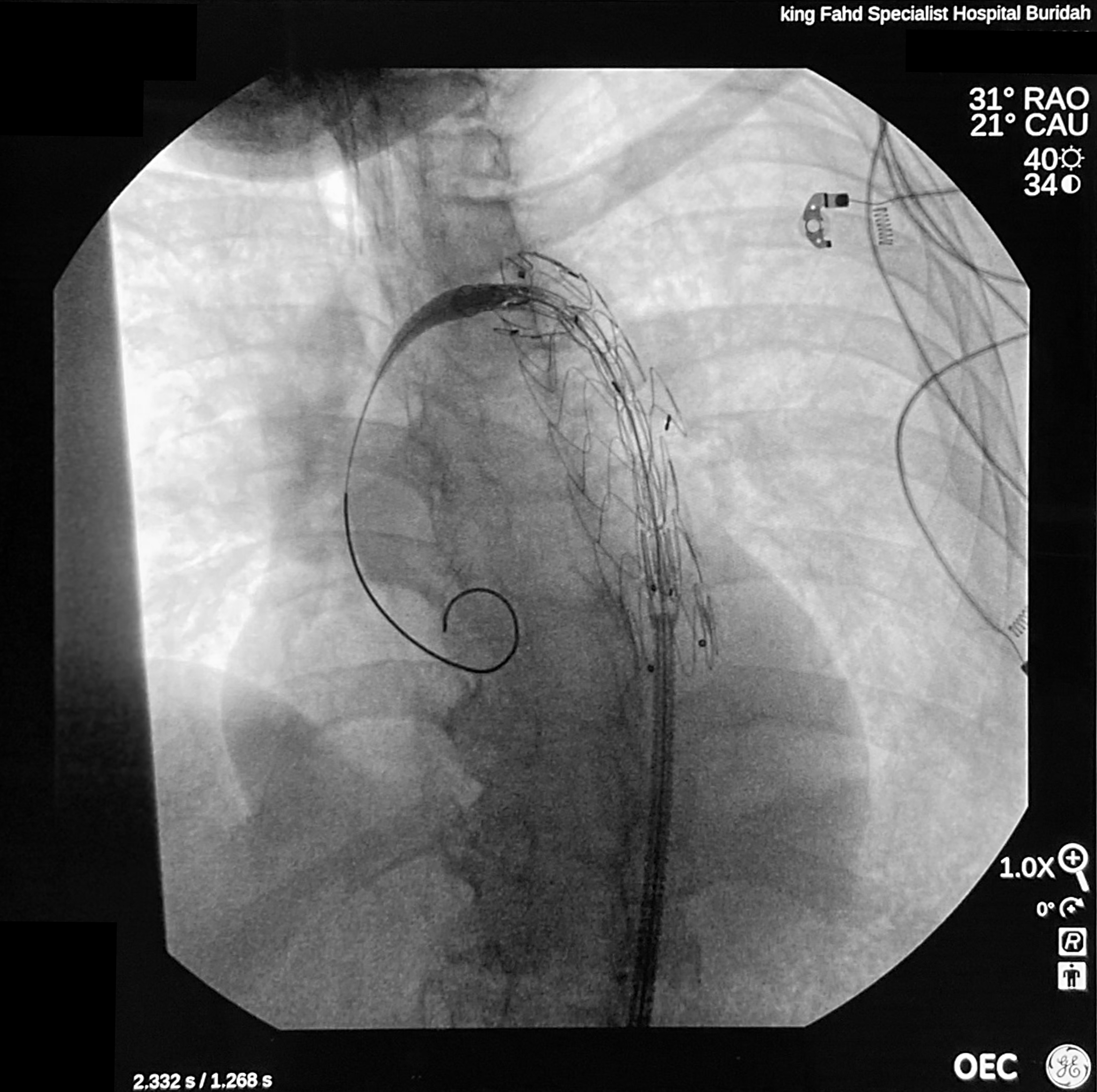
8. Dynamic fluoroscopic images during the placement of the second stent graft inside the first stent graft to correct the endoleak.
9. Digital Subtracted Angiography (left image), non-subtracted fluoroscopic image (right image): confirmation of the placement of the second stent graft showing exclusion of both the aneurysm and the endoleak from the aneurismal sac – acquisition performed in left oblique view of about 30 degrees and caudal angulation of 10 degrees.
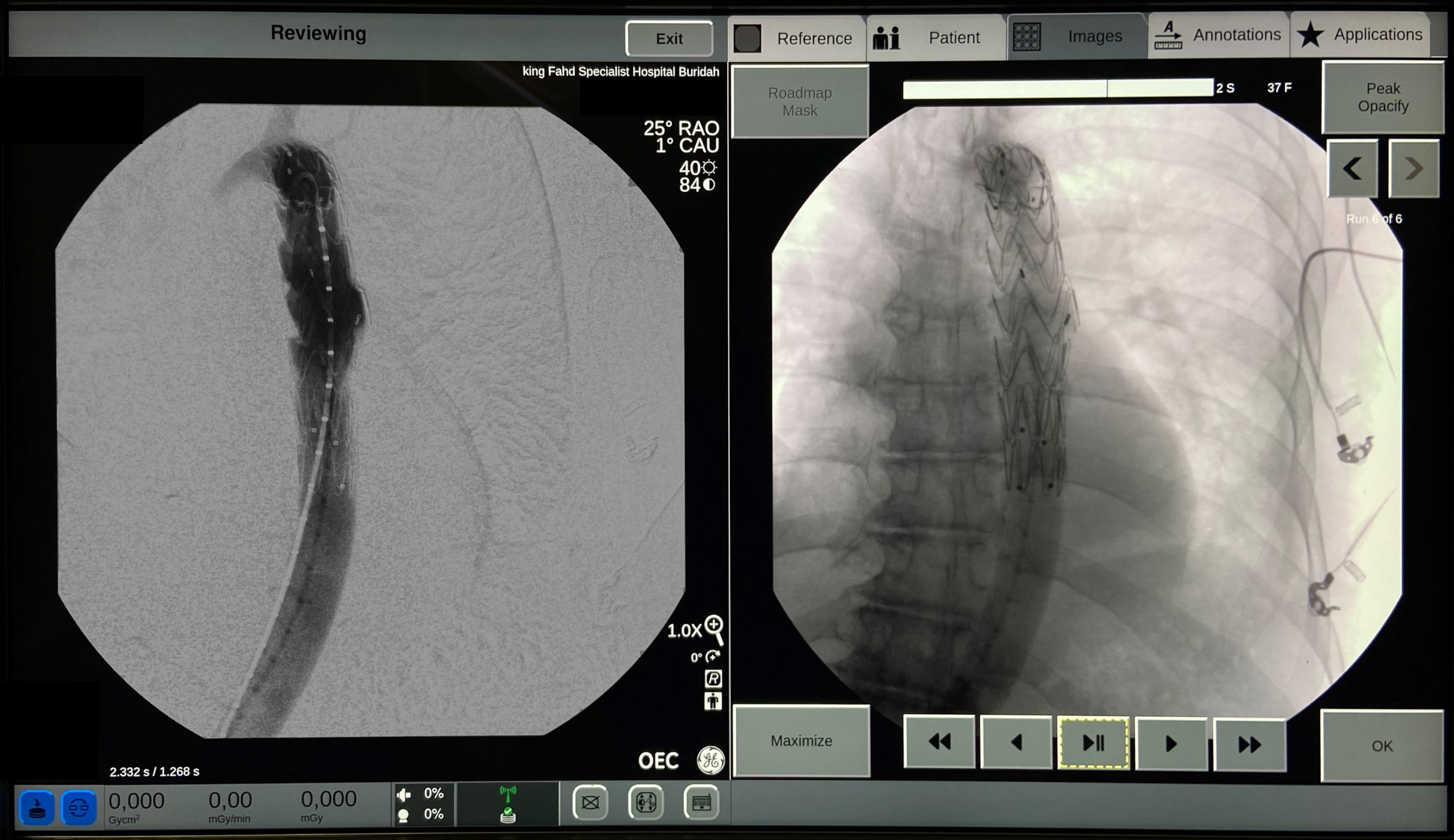
10. Digital Subtracted Angiography (left image), non-subtracted fluoroscopic image (right image): final control of the procedure showing exclusion of the aneurysmal sac from the blood circulation – acquisition performed in right oblique view of 25 degrees.
The statements by GE’s customers described here are based on their own opinions and on results that were achieved in the customer’s unique setting. Since there is no “typical” hospital and many variables exist, i.e. hospital size, case mix, etc.. there can be no guarantee that other customers will achieve the same results. JB04059UK