Minimally Invasive Outpatient Spine Surgery with OEC 3D
Interview with Dr. Ernest E. Braxton Jr. Neurosurgeon at Vail-Summit Orthopaedics & Neurosurgery in Vail, Colorado, United States.
Vail-Summit Orthopaedics and Neurosurgery is a 13-physician group practice specializing in musculoskeletal care, sports medicine, joint reconstruction, spine surgery, as well as physiatry and rehabilitation.
Why minimally invasive outpatient spine surgery?
I started my career doing about 60% cranial work, skull-based work, tumors, cerebrovascular and about 40% of spine, mostly complex spine and in trauma situations. Then, I made a little pivot towards minimally invasive spine with an emphasis on outpatient surgery. There are a lot of similarities between the population that I see here in Vail and in the military. They are for the most part, very healthy, active, and motivated patients, looking for a quick recovery. It seemed to make more sense to perform minimally invasive operations where there is less tissue disruption and do the procedure in a way that it could be outpatient. The COVID pandemic really highlighted that and was an accelerant to helping us do more outpatient surgeries because we needed the hospital beds to reserve them for higher acuity patients. Yet, patients with elective degenerative problems really wanted to get their procedures done, and in an outpatient setting where they can recover at home.
Why did you choose the OEC 3D for your practice?
We did an exhaustive search trialing and looking at other C-arms. At the end of the day, one of my concerns was what is the long-term durability of the product? What if the technology shifts or moves, will this C-arm still be competitive? Will this still meet my surgical needs for my patients?
The fact that the OEC 3D is open source*, it means that you can apply many different types of implants and technologies. This gives me, as a surgeon, a lot more options when discussing alternatives with a patient.
What type of procedures are you using the OEC 3D C-arm for?
The OEC 3D has really been a game changer in my practice. We use the OEC 3D for artificial disc replacement surgery, both in the cervical and lumbar spine, spine arthrodesis or spine fusion operations, for lumbar discectomy and laminectomy, as well as neuromodulation cases where implanting spinal cord stimulators.
One of the more challenging cases we do is localizing in the thoracic spine. We don’t have the same landmarks as in the cervical spine or lumbar spine, and when I’m doing thoracic procedures, I find the OEC 3D a must have device. In fact, we make it a note that the OEC 3D needs to be in the room, or we don’t do the case. Having the large field of view and being able to get a 3D reconstruction when you’re in the thoracic spine is critical.
The OEC 3D has a small footprint and less radiation exposure: We’re not leaving the room to do a spin or a 3D reconstruction, and when it is not necessary to do a 3D reconstruction, we use the OEC 3D as a conventional C-arm, with a large field of view.
How does the OEC 3D improve your workflow?
I thought the OEC 3D was a conventional C-arm. I didn’t realize that it had the ability to obtain 3D reconstructed images of the spine for surgery. The OEC 3D offers different methods of imaging specific anatomy, and it has features that I wasn’t used to having but found to be invaluable, like the Live View camera and the green laser aimer.
Specifically during neuromodulation case or spinal cord similar case, where the precise localization of your leads is critical to the outcome of the surgery.
With other traditional C-arms, what we had to do was to take a shot and then move the detector along as we were driving the lead along the spinal cord.
What has changed our workflow in multiple ways is the 3D acquisition time. When I was using other devices, often we would skip the post-op spin because of radiation exposure to the patient and added surgical time. Now, with the OEC 3D system, we do pre and post-spins for every case because the imaging is superb, the timing is quick, then the question is, why wouldn’t you get a second spin?
When placing an artificial disk, unlike a conventional fusion operation, it’s important to know exactly where you are, to be precisely in the midline and make sure that the prosthetic fits the patient perfectly. With the OEC 3D, having the capability to get a 3D spin, we’re able to get better matches of the prosthetic and the patient anatomy, and know before leaving the operating room that the prosthetic is well placed.
The OEC 3D augmented what we already can do, because at the end of the day, we really need to know in real time where we’re at anatomically.
Navigation provides us a picture of the spine, in my case, 20 minutes or an hour ago; then, when I need to refresh that, getting a new spin or refreshing that image can be done in less than 3 minutes.
OEC 3D enables us to check the precise location of the instrumentation prior to closing, and because of the efficiency, the OEC 3D has allowed us to do more cases.
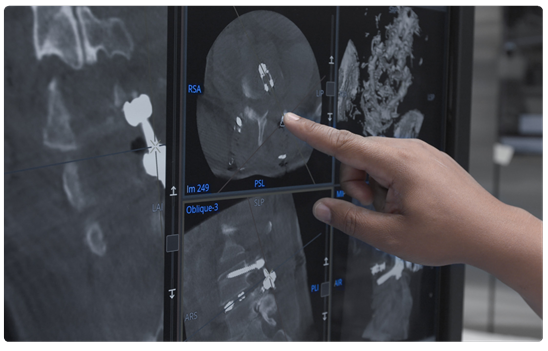
Review of spine images on OEC 3D Volume Viewer.
Dr. Braxton preparing for a 3D acquisition using OEC 3D assistant for collision check.
Why choose the OEC 3D over other C-arms?
One of the first things I noticed when comparing the OEC 3D to other 3D C-arms is the smaller footprint, the speed of image acquisition, and decreased radiation exposure, both to the patient and to the surgical team.
My favorite feature is the motorized position memory recall. When I line up a view to a pedicle or a specific part of the anatomy, I’ll ask the technologist to save that shot, save that position, and then I’ll go to another position. Later, the technologist can automatically go back to the last position quickly and easily. That is one of the biggest frustrations that we had before having the OEC 3D, finding that last view that we had 10 minutes ago.
Initially, I was concerned about not being able to physically move the C-arm around the patient and about the learning curve that would take for the technologist, myself, and our surgical team to use the device. But I found there’s a lot of advantages to having a motorized C-arm, being able to memorize certain positions and coming back to those quickly, has really made my operations efficient.
What advice would you give to other surgeons that are purchasing
a 3D C-arm?
If there are surgeons who have reservations about considering the OEC 3D C-arm, especially in an ASC, I would highly encourage them to do a trial of the device to see if it meets their needs for image quality. I think they’ll find that it’s a fiscally responsible decision, and it is a lighter footprint, smaller device to use in sometimes crammed operating rooms in surgery centers.
I can’t really think of a procedure where I would not want to have the OEC 3D. We have really fully incorporated the OEC 3D into our practice.
REFENCES
*OEC Open is the OEC 3D C-arm interface designed to transfer 3D reconstructed volume data set to navigation or robotic systems.
Dr. Ernest Braxton is a paid consultant for GE HealthCare and was compensated for his participation in this testimonial. The statements by Dr. Braxton described here are based on his own opinions and results that were achieved in his unique setting. Since there is no “typical” hospital and many variables exist, i.e. ambulatory surgery center size, case mix, etc. There can be no guarantee that other customers will achieve the same results. JB251a92XX