The renal system is known for its exquisitely sensitive nature.
Operating under finely-tuned conditions, the kidneys constantly juggle an array of core functions. All day they filter toxins, maintain acid-base balance and regulate blood pressure, to name but a few.1
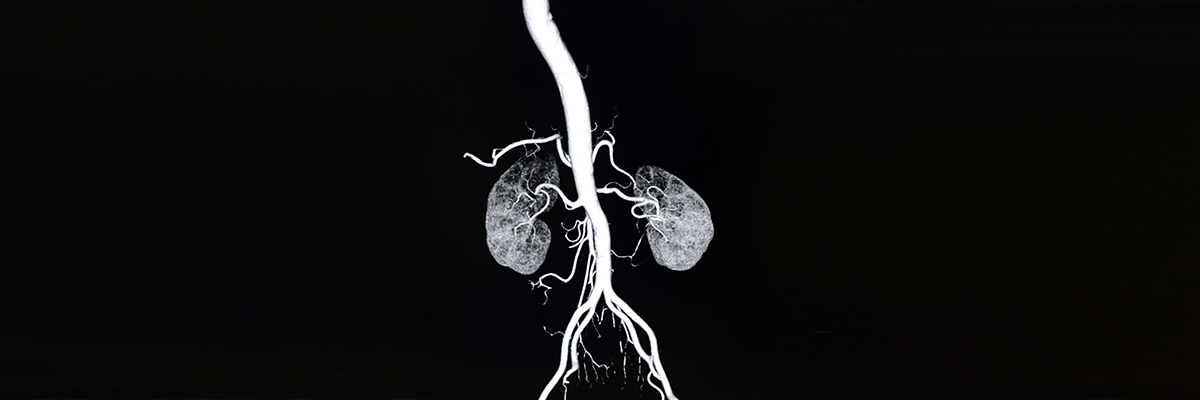
To sustain all this metabolic activity, a certain amount of blood needs to pass through the renal system at all times. For rather small organs, the kidneys command a hefty 20% of cardiac output every minute.2
Even in healthy kidneys, homeostasis is a precarious matter. This is partly a quirk of renal anatomy. The inner regions of each kidney are penetrated by over one million nephrons (functional units).1 With nephrons running alongside unusually long capillaries, any insults to blood flow (e.g. dehydration) may result in ischaemic injury.3 In vulnerable populations with underlying comorbidities, the kidneys may also become more susceptible to such insults.
Damage can occur in about 50% of nephrons before there are changes in the markers of kidney function, such as serum creatinine or glomerular filtration rate (GFR).4 This is due to renal functional reserve (RFR). RFR represents the capacity of the kidneys to increase GFR in response to certain physiological or pathological triggers. However, when RFR is impaired – as in conditions such as diabetes mellitus and CKD – there is less ability to bounce back, or compensate.5 Over time this means repeated renal injuries are likely to injure even more nephrons, further eroding renal function.4
In this context, iodinated contrast agents add a unique challenge to the already intense workload of the vulnerable kidney. Iodine itself is directly chemotoxic to renal tubular cells, but healthy patients have a robust repair capacity.4,6 With less reserve comes an impaired ability to regenerate tubular epithelial cells.4
The iodine-based contrast media are among the most widely used drug in the history of modern medicine.7 Delivered intravascularly, no other drug that reaches the kidney almost immediately is used in as high concentration or total dose.
Demand for their use only continues to grow in parallel with an ageing, increasingly multimorbid population.8,9 Cancer patients, for instance, are needing more contrast-enhanced CT scans despite their often blunted functional reserve.10 Complex intra-arterial procedures using high volumes of contrast are also becoming more routine.11
While the degree of causality has been disputed, there is certainly correlation between contrast volume and development of AKI, at least in those at high risk.12 As CKD progresses, for example, the incidence of acute kidney injury following PCI rises steeply, an occurrence strongly associated with in-hospital mortality.13
So asides from direct toxicity, why else might contrast agents carry this risk? The exact interplay of mechanisms is still being pieced together, but research has highlighted a few clues.14 To start with is the issue of microcirculation.
Of paramount importance in renal vasculature is a red blood cell’s ability to twist and deform so it can navigate capillaries.15 As mentioned, the descending capillaries are long and very narrow, making even subtle changes in flow significant.
Contrast agents which are hyperosmolar cause fluid to leave red blood cells, often distorting their typical biconcave shape.16 This manifests as a distinctly ‘spiky’ appearance under the microscope.17 There is evidence this translates to less elasticity, causing flow resistance in capillaries and, crucially, reduced oxygen delivery to renal cells.17
Caption: Coloured scanning electron micrograph (SEM) of a red blood cell travelling through a capillary
Iodinated contrast agents are also thought to impede blood flow by increasing blood viscosity18 and buckling endothelial cells so they protrude into blood vessels.19 Furthermore, they tend to tip the balance towards release of vasoconstrictors while limiting availability of the potent vasodilator nitric oxide.18 It is worth reiterating here that even healthy kidneys need an abundant blood supply to function properly.
Finally, there are the more direct osmotic effects. Following injection, contrast media are diluted in the bloodstream and then freely filtered into nephrons.20 With 99% of filtrate reabsorbed, their concentration rises 100-fold in the tubules; no other organ faces as much exposure to contrast media as the kidneys.14
While the kidneys try diluting contrast by ramping up sodium and water excretion, the side effect is a surge in hydrostatic pressure.21 This can lower filtration pressure - and hence renal function - precisely when tubular cells are working harder to cope with the added pressure.
Ultimately, the relationship between contrast and acute kidney injury is a nuanced one.
The understandable difficulty of designing ethically sound in vivo studies makes determining causality a challenge and while correlation has been revealed consistently, some have brought up the issue of confounding factors.12
Yet as discussed, a mounting body of theory and observational data warrants ongoing caution. And with the number of vulnerable patients encountering Radiologists and Interventionalists set to rise, caution may give the delicate kidneys their best chance at thriving.
Want to find out more about GE Healthcare contrast media?
[Click here] to visit the product promotional site
Abbreviations
AKI: acute kidney injury
CKD: chronic kidney disease
CT: computed tomography
PCI: percutaneous coronary intervention
References
1. Amerman E. Human Anatomy & Physiology. Harlow: Pearson Education, 2015: 941-83.
2. Mullens W , Nijst P . J Am Coll Cardiol 2016; 67(19): 2209-12.
3. Sadat U, ISRN Radiol 2013; 496438.
4. Sharma A et al. Nephron Clin Pract 2014; 127(1-4): 94-100.
5. McCullough PA et al, J Am Coll Cardiol 2016; 68(13): 1465-73.
6. Seeliger E et al. Eur Heart J 2012; 33(16): 2007-15.
7. Christiansen C. Toxicology 2005; 209: 185-7.
8. Grand View Research. Available at: https://www.grandviewresearch.com/press-release/global-contrast-
media-contrast-agents-market, Accessed on 28.10.20
9. Kingston A et al. Age Ageing 2018; 47(3): 374-80.
10. Hong SI et al. Support Care Cancer 2016; 24(3): 1011-7.
11. Keuffel E et al. J Med Econ 2018; 21: 356-64.
12. Azzalini L et al. Can J Cardiol 2017; 33(10): 1225-8.
13. Tsai TT et al. JACC Cardiovasc Interv 2014; 7(1): 1-9.
14. Hiremath S, Velez JCQ. Curr Opin Nephrol Hy 2019; 29: 152-60.
15. Kerl JM et al. Acta Radiol 2008; 49(3): 337-43.
16. Widmark JM. Proc (Bayl Univ Med Cent) 2007; 20(4): 408-17.
17. Jung F et al. Clin Hemorheol Micro 2008; 38(1): 1-11.
18. Mehran R et al. New Engl J Med 2019; 380(22): 2146-55.
19. Franke RP et al. Clin Hemorheol Micro 2011; 48(1): 41-56.
20. Andreucci M et al. Drug Healthc Patient Saf 2017; 9: 25-37.
21. Berg KJ. Scand J Urol Nephrol 2000; 34(5): 317-322.
02-2021 JB00309UK